ADHD: More Common Than Depression in Child Suicide
Homecoming Issue
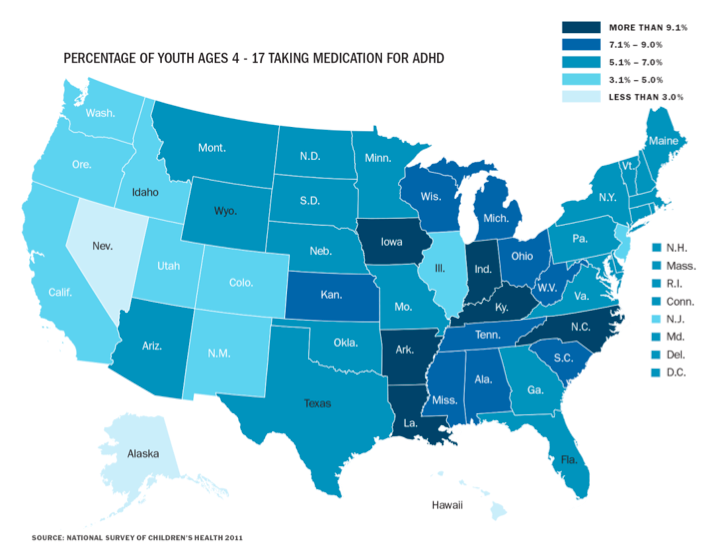
Map showing the percentage of youth ages 4-17 taking medication for ADHD as of 2011.
October 21, 2016
With child suicide plaguing far too many young Americans, it is important to recognize its causes. New research released in September 2016 shows that children who commit suicide are less likely to have depression and more likely than their peers to have attention-deficit disorder (ADD) or attention-deficit/hyperactivity disorder (ADHD). Typically, “children under the age of 12 are overlooked or forgotten in conversations discussing suicide and prevention of suicide.” In reality, a small amount of children in the United States between age 5 and 11 kill themselves each year — most of them lived with ADHD/ADD more than any other mental health diagnosis including depression. Databases tracking violent deaths showed that among suicide decedents with known mental health problems, young children aged 5 to 11 years were more likely to experience ADD/ADHD and less likely to experience depression/dysthymia compared with children and adolescents aged 12 to 14 years.
These findings raise questions for many about impulsive response to psychosocial adversity in younger suicide decedents, and they suggest a need for both common and developmentally-specific suicide prevention strategies during the elementary schools and early adolescent years.
So what do depression and ADD/ADHD look like? When someone is feeling depressed or down it doesn’t necessarily mean that the diagnosis of major depression would be appropriate. It is important to recognize that what is required for the clinical diagnosis of depression is the presence of a collection of different symptoms. According to DSM-IV, the publication of the American Psychiatric Association, the symptoms of major depression are: depressed mood most of the day, nearly every day (in children and teens, this can be irritable mood rather than depressed), loss of interest or pleasure in all, or almost all, activities, significant weight loss (when not dieting) or weight gain, a significant change in appetite, insomnia or hypersomnia (i.e. sleeping too much) nearly every day, extreme restlessness or lethargy, fatigue or loss of energy nearly every day, feelings of worthlessness or inappropriate guilt, diminished ability to think or concentrate nearly every day, and recurrent thoughts of death and/or suicidal thoughts. Around five of those symptoms must be present during a consistent two week period in order for one to be diagnosed with depression.
Research also shows that the core symptoms for depression in children and adolescents are the same in adults. This newfound research suggests that depression found in children with ADHD/ADD is not from the result of demoralization that ADHD/ADD can cause. Although such struggles may be an important risk factor in the development of depression in children with ADD/ADHD, more likely, the depression found in these children is a distinct disorder and not demoralization.
Lead author Arielle H. Sheftall, PhD, from Nationwide Children’s Hospital, Columbus, Ohio, explained to Medscape Medical News, “The major message of the study is that the circumstances preceding suicide in children are, to a large extent, similar to those for suicide in early adolescents, with a few key exceptions that tend to fall along developmental lines.”
New research shows that children who died by suicide were most commonly male, black, died by hanging/strangulation/suffocation, died at home, and experienced relationship problems with family members and friends. Children were also less likely to leave a suicide note, be depressed, or experience boyfriend/girlfriend problems in comparison to early adolescents who died by suicide.
The Signs of Suicide prevention program is one shown to be effective in reducing self-reported suicidal behavior in middle and high school children. They raise awareness that suicide is a risk for some mental health disorders, especially depression, and teach how to act and recognize when someone is displaying warning signs related to suicidal thoughts and behaviors.